
AVIPTADIL
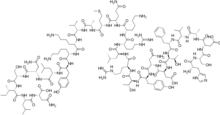
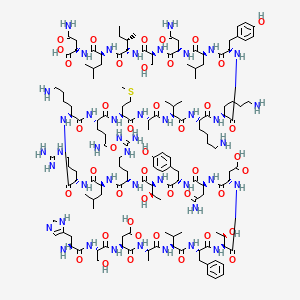
- Molecular FormulaC147H237N43O43S
37221-79-7[RN]
6J2WVD66KR
L-Asparagine, L-histidyl-L-seryl-L-α-aspartyl-L-alanyl-L-valyl-L-phenylalanyl-L-threonyl-L-α-aspartyl-L-asparaginyl-L-tyrosyl-L-threonyl-L-arginyl-L-leucyl-L-arginyl-L-lysyl-L-glutaminyl-L-met hionyl-L-alanyl-L-valyl-L-lysyl-L-lysyl-L-tyrosyl-L-leucyl-L-asparaginyl-L-seryl-L-isoleucyl-L-leucyl-
Vasoactive intestinal octacosapeptide
Invicorp (aviptadil + phentolamine)
(2S)-4-amino-2-[[(2S)-2-[[(2S,3S)-2-[[(2S)-2-[[(2S)-4-amino-2-[[(2S)-2-[[(2S)-2-[[(2S)-6-amino-2-[[(2S)-6-amino-2-[[(2S)-2-[[(2S)-2-[[(2S)-2-[[(2S)-5-amino-2-[[(2S)-6-amino-2-[[(2S)-2-[[(2S)-2-[[(2S)-2-[[(2S,3R)-2-[[(2S)-2-[[(2S)-4-amino-2-[[(2S)-2-[[(2S,3R)-2-[[(2S)-2-[[(2S)-2-[[(2S)-2-[[(2S)-2-[[(2S)-2-[[(2S)-2-amino-3-(1H-imidazol-5-yl)propanoyl]amino]-3-hydroxypropanoyl]amino]-3-carboxypropanoyl]amino]propanoyl]amino]-3-methylbutanoyl]amino]-3-phenylpropanoyl]amino]-3-hydroxybutanoyl]amino]-3-carboxypropanoyl]amino]-4-oxobutanoyl]amino]-3-(4-hydroxyphenyl)propanoyl]amino]-3-hydroxybutanoyl]amino]-5-carbamimidamidopentanoyl]amino]-4-methylpentanoyl]amino]-5-carbamimidamidopentanoyl]amino]hexanoyl]amino]-5-oxopentanoyl]amino]-4-methylsulfanylbutanoyl]amino]propanoyl]amino]-3-methylbutanoyl]amino]hexanoyl]amino]hexanoyl]amino]-3-(4-hydroxyphenyl)propanoyl]amino]-4-methylpentanoyl]amino]-4-oxobutanoyl]amino]-3-hydroxypropanoyl]amino]-3-methylpentanoyl]amino]-4-methylpentanoyl]amino]-4-oxobutanoic acid

Aviptadil Acetate
CAS#: 40077-57-4 (free base)
Chemical Formula: C155H253N43O51S
Exact Mass:
Molecular Weight: 3567.039
H-His-Ser-Asp-Ala-Val-Phe-Thr-Asp-Asn-Tyr-Thr-Arg-Leu-Arg-Lys-Gln-Met-Ala-Val-Lys-Lys-Tyr-Leu-Asn-Ser-Ile-Leu-Asn-NH2 tetraacetic acid.
Aviptadil had been in phase II clinical trials for the treatment of pulmonary arterial hypertension and idiopathic pulmonary fibrosis. But these researches were discontinued in 2011.
In 2006, Orphan Drug Designations were granted in the E.U. for the treatment of pulmonary arterial hypertension, and sarcoidosis and acute lung injury in 2006, and 2008, respectively.
The compound was co-developed by Lung Rx (subsidiary of United Therapeutics) and Mondobiotech.
Aviptadil (INN) is an injectable synthetic formulation of human vasoactive intestinal peptide (VIP).[1] VIP was discovered in 1970, and has been used to treat various inflammatory conditions, such as acute respiratory distress syndrome (ARDS), asthma and chronic obstructive pulmonary disease (COPD).
| Clinical data | |
|---|---|
| Trade names | RLF-100 / Zyesamiô |
| AHFS/Drugs.com | International Drug Names |
| ATC code | none |
| Identifiers | |
| showIUPAC name | |
| CAS Number | 40077-57-4 |
| PubChem CID | 16132300 |
| ChemSpider | 17288959 |
| UNII | A67JUW790C |
| KEGG | D12127 |
| ChEMBL | ChEMBL2106041 |
| CompTox Dashboard (EPA) | DTXSID7048584 |
| Chemical and physical data | |
| Formula | C147H237N43O43S |
| Molar mass | 3326.83 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| showSMILES | |
| showInChI | |
| (what is this?) (verify) |
Regulatory history
ARDS in COVID-19
Studies have found that aviptadil may be beneficial for severely ill patients with COVID-19 related ARDS.[2] ACTIV-3, a trial examining aviptadil acetate (Zyesami), is recruiting patients as of 2 July 2021.[3] A separate trial is examining inhaled aviptadil for patients with high risk for ARDS, is ongoing as of 21 May 2021.[4] A trial for intravenous aviptadil for the same indication concluded in February 2021.[5]
U.S.-Israeli NeuroRx Inc partnered with Relief Therapeutics to develop aviptadil in the United States. In June 2020, the U.S. Food and Drug Administration granted fast-track designation to aviptadil for treatment of respiratory distress in COVID-19.[6] In September 2020, NeuroRX submitted a request for an Emergency Use Authorization to the US FDA for its use in patients in intensive care.[7] May 2021: NRx Pharmaceuticals Announces Positive Results for ZYESAMI (Aviptadil-acetate) and Submits Emergency Use Authorization Application to USFDA to Treat Critical COVID-19 in Patients Suffering from Respiratory Failure.[8]
(Aviptadil-acetate) and Submits Emergency Use Authorization Application to USFDA to Treat Critical COVID-19 in Patients Suffering from Respiratory Failure.[8]
Jan, 2021: Zuventus healthcare Ltd seeks approval for Aviptadil from India’s drug controller for emergency use in COVID-19 treatment. Mumbai’s Zuventus healthcare Ltd. has got the nod to conduct Phase 3 clinical trials of Aviptadil injectable formulation. The SEC noted that Zuventus had presented revised Phase 3 clinical trial protocol before the committee, and after “detailed deliberation”, it recommended grant of permission of Phase 3 trials with the drug.[9] [10]
Aviptadil/phentolamine combination for Erectile Dysfunction (ED)
October 2000 UK (Invicorp): Aviptadil, an injectable formulation of vasoactive intestinal polypeptide (VIP) in combination with the adrenergic drug phentolamine is approved as an effective alternative therapy for erectile dysfunction (ED) patients. 1 dose intracavernosal injection contains 25 micrograms aviptadil and 2 mg of phentolamine mesilate for the treatment of erectile dysfunction. Aviptadil dose used for treatment of erectile dysfunction is far lesser as compared to dose used for the treatment of ARDS.[11][12]
Vasoactive intestinal peptide (VIP)
Vasoactive intestinal peptide (VIP) is a 28-residue amino acid peptide first characterized in 1970 that was initially isolated from porcine duodenum. A member of the secretin/glucagon hormone superfamily. VIP was initially discovered owing to its potent vasodilatory effects (as its name implies). VIP is widely distributed in the central and peripheral nervous system as well as in the digestive, respiratory, reproductive, and cardiovascular systems as a neurotransmitter and neuroendocrine releasing factor. These effects contribute to an extensive range of physiological and pathological processes related to development, growth, and the control of neuronal, epithelial, and endocrine cell function.[13]
VIP Receptors
VIP acts on two receptors – VPAC1 and VPAC2, which are class B of G-protein-coupled receptors (GPCRs).VPAC1 is mainly present in the lung and T-lymphocytes, whereas VPAC2 is mainly seen in the smooth muscle,mast cells and the basal parts of the lung mucosa.[14]
Expression of VIP
VIP is produced in the neurons in the central and peripheral nervous systems. VIP is mainly localized in the myenteric and submucosal neurons and nerve terminals in the GI tract. Endogenous VIP is released by numerous stimuli such as acetylcholine (ACh), ATP, serotonin (5-HT), substance P (SP), GLP-2 from at least two populations of VIP-positive nerves: cholinergic and non-cholinergic VIP-releasing nerves. In guinea pig small intestine, most VIP-positive nerves in the mucosa and submucosa are non-cholinergic secretomotor neurons and well colocalized with neuronal nitric oxide synthase (nNOS) in human colonic circular muscles. VIP is also expressed in immune cells, such as activated T cells and therefore present in lymphoid tissues including Peyer’s patches, the spleen, and lymph nodes, in addition to the VIP-ergic innervation in lymphoid tissues. Beside the neuronal source, VIP is also expressed and released from endocrine organs – Heart, Thyroid, Kidney and GI tracts.[15]
Localization of VIP
- VIP is highly localised in lungs (70%) and binds with alveolar type II (AT II) cells via VPAC1.[2] The biological (vasodilator) activity of vasoactive intestinal peptide (VIP) was discovered in the lungs before the peptide was isolated and chemical identity characterized from intestine. Although VIP levels are consideralbly high in the brain or gut:VIP is localized in key sites in the lung, has potent activities on its major functions, and appears to play an important role in pulmonary physiology and disease.[16]
- The principal localization of VIP-containing neurons in the tracheobronchial tree is in the smooth muscle layer, around submucosal mucous glands and in the walls of pulmonary and bronchial arteries. Immunoreactive VIP is also present in neuronal cell bodies forming microganglia that provide a source of intrinsic innervation of pulmonary structures.[16]
Vasoactive Intestinal Peptide (VIP) and SARS-CoV-2
VIP is highly localised in lungs and binds with alveolar type II (AT II) cells via VPAC1 receptor. AT II cells constitute only 5% of pulmonary epithelium. Angiotensin Converting Enzyme 2 (ACE 2) surface receptors arepresent in AT II cells. AT II cells produces surfactant and plays an important role in the maintenance of type 1epithelial cells. SARS-CoV-2 enters into AT II cells by binding to ACE 2 surface receptors with its spike protein. SARS CoV-2 attack mainly type II cells (not type I alveolar cells) and results in the death of alveolar type II (AT 11) cells which produces surfactant, resulting in[2]
- Profound defect in oxygenation
- Leading to hypoxia
Mechanism of action of Aviptadil
- Pulmonary alveolar type II Cells have a high concentration of ACE 2 receptors on their cell membrane
- Investigators have confirmed that the SARS-CoV family of viruses selectively attack pulmonary Alveolar Type II (ATII) cells because of their ACE2 receptors, in contrast to other pulmonary epithelial cells.
- SARS-CoV Viruses bind to ACE2 receptors in order to enter the cell. Viral replication and rupture liberates inflammatory cytokines and destroys surfactant production
- VIP binds uniquely to receptors on Alveolar Type II cells in the lung, the same cells that bind the SARS-CoV-2 virus via their ACE2 receptors
- VIP is heavily concentrated in the lung and binds specifically to VIP receptors on alveolar type II cells. VIP exerts a broad anti-cytokine effect on immune system cells
- VIP specifically upregulates surfactant production via upregulation of C-Fos protein and protects type II cells from cytokine
- Upregulating the production of surfactant, the loss of which is increasingly implicated in COVID-19 respiratory failure [17]
Aviptadil a synthetic form of VIP results in rapid clinical recovery in patients with SARS-CoV-2 infection.[2]
Effect of Aviptadil on Lungs in COVID-19
Preservation of Pulmonary Tissue
Preserving surfactant production in the lung and in protecting type 2 alveolar cells. Significantly delayed the onset of edematous lung injury, effective in preventing ischemia-reperfusion injury, Prevents NMDA-induced caspase-3 activation in the Lung.[18]
Inhibits alveolar epithelial cell Apoptosis
VIP is a proven inhibitor of activation-induced perforin, as well as of granzyme B and therefore actively contributes to the reduction of deleterious proinflammatory and cell death-inducing processes, particularly in the lungs. Aviptadil restores barrier function at the endothelial/alveolar interface and thereby protects the lung and other organs from failure.[18]
VIP Promotes synthesis of pulmonary surfactant
Studies have demonstrated that VIP binds on type II cells and increases the incorporation of methyl-choline into phosphatidylcholine – the major component of the pulmonary surfactants by enhancing the activity of the enzyme choline-phosphate cytidylyltransferase. VIP upregulates C-Fos protein expression in cultured type II alveolar cells, which is instrumental in promoting synthesis of pulmonary surfactant phospholipids (Li 2007) and induces surfactant protein A expression in ATII cells through activation of PKC/c-Fos pathway.[18]
VIP decreases Pulmonary Inflammation
Anti-cytokine effect- Inhibits IL-6,TNF-α production and inhibit NF-kB activation. Protects against HCl-induced pulmonary edema.[18]
Pharmacokinetic Properties
Half-life: Its plasma half-life of elimination is 1 to 2 minutes.[2] Metabolism/Distribution: After injection of 1 µg radioactively labelled Aviptadil as bolus to patients a very rapid tissue distribution was observed Within 30 min about 45% of the radioactivity was found in the lungs Over an observation period of 24 hrs only minimal activity was detected in the GI tract & almost no activity was found in the liver or spleen Radioactivity in the lungs decreased within four hours to 25% and within 24 hours to 10% Apparent volume of distribution: Aviptadil has a volume of distribution of 14 ml/kg.[2] Tissue Distribution:Aviptadil binds to its receptors in discrete locations within the gastrointestinal, respiratory, and genital tracts. Aviptadil is localized on respiratory epithelium, smooth muscles of the airways, blood vessels and alveolar walls. Elimination:After injection of radiolabelled Aviptadil radioactivity was almost completely eliminated by the kidneys, 35% within 4 hours, and 90% within 24 hours
Justification for Aviptadil use in the treatment of ARDS
COVID-19-related death is primarily caused by Acute Respiratory Distress Syndrome (ARDS). The trigger for ARDS is widely attributed to a cytokine storm in the lungs, in which the virus causes release of inflammatory cytokines. As a result, alveolae of the lungs fill with fluid and become impermeable to oxygen, even in the setting of mechanical ventilation. SARS-CoV-2 is known to cause respiratory failure, which is the hallmark of Acute COVID-19. Tragically, survival of patients with COVID-19 who progress to Acute Respiratory Distress is dismal. There is an urgent need for a treatment approach that goes right into the heart of the matter – the alveolar type 2 cells which are vulnerable entry points and hosts for the SARS-CoV-2 virus.[19]
Aviptadil-Evidence from Studies in ARDS
Phase III Study-Increased Recovery and Survival in Patients With COVID-19 Respiratory Failure Following Treatment with Aviptadil
A multicenter, randomized, placebo-controlled trial in 196 patients with PCR+ COVID-19 receiving intensive care at 10 U.S. hospitals – 6 tertiary care and 4 regional hospitals to determine whether intravenous aviptadil (synthetic VIP) is superior to placebo in achieving recovery from respiratory failure and survival at 60 days post treatment. Primary, prespecified endpoint was “alive and free from respiratory failure at day 60.” Across all patients and sites of care, patients treated with aviptadil were significantly more likely to be alive and free from respiratory failure at 60 days, compared to those treated with placebo (P=.02) and demonstrated improvement in survival alone (P<.001). Advantages in survival for aviptadil-treated patients were seen in both the subgroup classified as 2 on the National Institute of Allergy and Infectious Disease (NIAID) ordinal scale (58.6% vs. 0%; p=.001) and the NIAID=3 subgroup (83.1% vs. 62.8%; p=.03). Among patients who recovered successfully, those treated with Aviptadil had a median 10-day reduction in length of hospital stay compared to placebo patients (P=.025). Treatment with aviptadil demonstrates multi-dimensional efficacy in improving the likelihood of recovery from respiratory failure and survival to 60 days, and markedly reduced hospital stay in critically ill patients with respiratory failure caused by COVID-19.[20]
Case report: Rapid Clinical Recovery from Critical COVID-19 Pneumonia with Aviptadil
A 54 year old man with double lung transplant presented with headache, fever and productive cough. COVID-19 infection was confirmed by positive RT-PCR of nasopharyngeal swab. The patient required only supportive care for 3 days and was discharged home. Two weeks later he presented with worsening dyspnea, fever and severe hypoxemia requiring high flow O2 and ICU admission. Chest CT showed diffuse bilateral consolidations. He had markedly elevated inflammatory markers. He was treated with dexamethasone and tocilizumab without improvement. He was not a candidate for Remdesivir due to chronic kidney disease. Convalescent plasma was not available, Pro-BNP level was normal; echocardiogram showed preserved biventricular function. He received Aviptadil, a total of three doses, per an open label access under an emergency use approved by USFDA. Rapid improvement in oxygenation and radiologic findings were noticed. No adverse effects were recorded. Patient was transferred out of the ICU 24 hours following the third dose and discharged home on room air 15 days later. This case report of lung transplant recipient with critical COVID-19 pneumonia treated with Aviptadil demonstrates rapid clinical and radiologic improvement.This is consistent with that VIP protects ATII cells, ameliorating the inflammation and improving oxygenation in critical COVID-19 pneumonia.[21]
Posology and method of administration
Aviptadil intravenous infusion is administered by infusion pump in escalating doses for 3 successive days
- Day 1 : Aviptadil 0.166 mcg/kg/hr (equivalent to 1 vial of Aviptadil Injection)
- Day 2 : Aviptadil 0.332 mcg/kg/hr (equivalent to 2 vials of Aviptadil Injection)
- Day 3 : Aviptadil 0.498 mcg/kg/hr (equivalent to 3 vials of Aviptadil Injection)
Duration of infusion depends on the patient’s body weight
- Body weight < 60 kg – 14 hour infusions of Aviptadil at escalating doses on 3 successive days
- Body weight 60 – 90 kg – 12 hour infusions of Aviptadil at escalating doses on 3 successive days
- Body weight > 90 kg – 10 hour infusions of Aviptadil at escalating doses on 3 successive days
Undesirable Effects
Gastrointestinal Disorders – Diarrhea, Vascular disorders – Hypotension, cutaneous flushing, facial flushing & Infusion related reactions[20]

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
References
- ^ Keijzers GB (April 2001). “Aviptadil (Senatek)”. Current Opinion in Investigational Drugs. 2 (4): 545–9. PMID 11566015. Archived from the original on 2010-09-02. Retrieved 2020-04-01.
- ^ Jump up to:a b c d e f Raveendran, A; Al Dhuhli, K.; Harish Kumar, G. (2021). “Role of Aviptadil in COVID-19”. BMH Medical Journal. 8 (2): 77-83.
- ^ National Institute of Allergy and Infectious Diseases (NIAID) (2021-06-25). “A Multicenter, Adaptive, Randomized, Blinded Controlled Trial of the Safety and Efficacy of Investigational Therapeutics for Hospitalized Patients With COVID-19”. International Network for Strategic Initiatives in Global HIV Trials (INSIGHT), University of Copenhagen, Medical Research Council, Kirby Institute, Washington D.C. Veterans Affairs Medical Center, AIDS Clinical Trials Group.
- ^ Leuppi, Jörg (2021-05-20). “Inhaled Aviptadil for the Treatment of COVID-19 in Patients at High Risk for ARDS: A Randomized, Placebo Controlled, Multicenter Trial”. Clinicaltrials.gov.
- ^ NeuroRx, Inc. (2021-02-23). “ZYESAMI (Aviptadil) for the Treatment of Critical COVID-19 With Respiratory Failure”. Lavin Consulting, LLC.
- ^ “Critically ill COVID-19 patients make quick recovery with treatment RLF-100”. New York Post. 2 August 2020. Retrieved 3 August 2020.
- ^ NeuroRx. “NeuroRx submits request for Emergency Use Authorization for RLF-100
![™]() (aviptadil) in the treatment of patients with Critical COVID-19 and Respiratory Failure who have exhausted approved therapy”. http://www.prnewswire.com. Retrieved 2020-09-24.
(aviptadil) in the treatment of patients with Critical COVID-19 and Respiratory Failure who have exhausted approved therapy”. http://www.prnewswire.com. Retrieved 2020-09-24. - ^ Pharmaceuticals, NRx. “NRx Pharmaceuticals Announces Positive Results for ZYESAMI
![™]() (Aviptadil-acetate) and Submits Emergency Use Authorization Application to USFDA to Treat Critical COVID-19 in Patients Suffering from Respiratory Failure”. http://www.prnewswire.com.
(Aviptadil-acetate) and Submits Emergency Use Authorization Application to USFDA to Treat Critical COVID-19 in Patients Suffering from Respiratory Failure”. http://www.prnewswire.com. - ^ Das, Sohini (2021-01-25). “Dr Reddy’s, Zuventus get nod to conduct Covid-19 trials on repurposed drugs”. Business Standard India.
- ^ SECmeeting, e COVID-19. “Recommendations of the SECmeeting to examine COVID-19 related proposals under accelerated approval process made in its 140thmeeting held on 18.01.2021 & 19.01.2021 at CDSCO, HQ New Delhi” (PDF). CDSCO. Retrieved 1 July 2021.
- ^ Keijzers, GB (April 2001). “Aviptadil (Senatek)”. Current Opinion in Investigational Drugs. 2 (4): 545–9. PMID 11566015.
- ^ Procivni, Aviptadil/phentolamine mesilate. “Scientific discussion” (PDF).
- ^ Iwasaki, M; Akiba, Y; Kaunitz, JD (2019). “Recent advances in vasoactive intestinal peptide physiology and pathophysiology: focus on the gastrointestinal system”. F1000Research. 8: 1629. doi:10.12688/f1000research.18039.1. PMC 6743256. PMID 31559013.
- ^ Mathioudakis, A; Chatzimavridou-Grigoriadou, V; Evangelopoulou, E; Mathioudakis, G (January 2013). “Vasoactive intestinal Peptide inhaled agonists: potential role in respiratory therapeutics”. Hippokratia. 17 (1): 12–6. PMC 3738270. PMID 23935337.
- ^ Iwasaki, M; Akiba, Y; Kaunitz, JD (2019). “Recent advances in vasoactive intestinal peptide physiology and pathophysiology: focus on the gastrointestinal system”. F1000Research. 8: 1629. doi:10.12688/f1000research.18039.1. PMC 6743256. PMID 31559013.
- ^ Jump up to:a b Said, Sami I. (June 1988). “Vasoactive Intestinal Peptide in the Lung”. Annals of the New York Academy of Sciences. 527 (1 Vasoactive In): 450–464. Bibcode:1988NYASA.527..450S. doi:10.1111/j.1749-6632.1988.tb26999.x. PMID 2898912. S2CID 26804295.
- ^ Javitt, Jonathan C (2020-07-25). “Vasoactive Intestinal Peptide treats Respiratory Failure in COVID-19 by rescuing the Alveolar Type II cell”. doi:10.22541/au.159569209.99474501. S2CID 221509046.
- ^ Jump up to:a b c d Javitt, Jonathan C (2020-05-13). “Perspective: The Potential Role of Vasoactive Intestinal Peptide in treating COVID-19”. doi:10.22541/au.158940764.42332418. S2CID 219771946.
- ^ “Relief Therapeutics and NeuroRx Announce Final Manufacturing Validation of RLF-100 for Phase 2b/3 Clinical Trial in Patients with COVID-19 Associated Acute Respiratory Distress Syndrome”. GlobeNewswire News Room. 2020-05-14.
- ^ Jump up to:a b Youssef, Jihad G.; Lee, Richard; Javitt, Jonathan; Lavin, Philip; Lenhardt, Rainer; Park, David J; Perez Fernandez, Javier; Morganroth, Melvin; Jayaweera, Dushyantha (2021). “Increased Recovery and Survival in Patients With COVID-19 Respiratory Failure Following Treatment with Aviptadil: Report #1 of the ZYESAMI COVID-19 Research Group”. SSRN 3830051.
- ^ Beshay, S.; Youssef, J.G.; Zahiruddin, F.; Al-Saadi, M.; Yau, S.; Goodarzi, A.; Huang, H.; Javitt, J. (April 2021). “Rapid Clinical Recovery from Critical COVID-19 Pneumonia with Vasoactive Intestinal Peptide Treatment”. The Journal of Heart and Lung Transplantation. 40 (4): S501. doi:10.1016/j.healun.2021.01.2036. PMC 7979412. S2CID 232282732.
//////////AVIPTADIL, RLF 100, DK 1000
CCC(C)C(C(=O)NC(CC(C)C)C(=O)NC(CC(=O)N)C(=O)O)NC(=O)C(CO)NC(=O)C(CC(=O)N)NC(=O)C(CC(C)C)NC(=O)C(CC1=CC=C(C=C1)O)NC(=O)C(CCCCN)NC(=O)C(CCCCN)NC(=O)C(C(C)C)NC(=O)C(C)NC(=O)C(CCSC)NC(=O)C(CCC(=O)N)NC(=O)C(CCCCN)NC(=O)C(CCCNC(=N)N)NC(=O)C(CC(C)C)NC(=O)C(CCCNC(=N)N)NC(=O)C(C(C)O)NC(=O)C(CC2=CC=C(C=C2)O)NC(=O)C(CC(=O)N)NC(=O)C(CC(=O)O)NC(=O)C(C(C)O)NC(=O)C(CC3=CC=CC=C3)NC(=O)C(C(C)C)NC(=O)C(C)NC(=O)C(CC(=O)O)NC(=O)C(CO)NC(=O)C(CC4=CN=CN4)N
